C3 glomerulopathy (C3G), a rare kidney disease, affects only two or three people out of every one million. That’s only a couple people out of the entire population of San Jose, California or Austin, Texas.
Although C3G only affects a select few, without treatment it can lead to severe kidney damage and failure, necessitating expensive dialysis or transplant. To date, there is no specific, effective therapy.
What is C3G?
C3 glomerulopathy is a relatively new classification. At a 2013 consensus meeting, scientists recommended that two rare diseases, dense deposit disease (DDD) and C3 glomerulonephritis (C3GN) be subgrouped under a new heading, C3G.
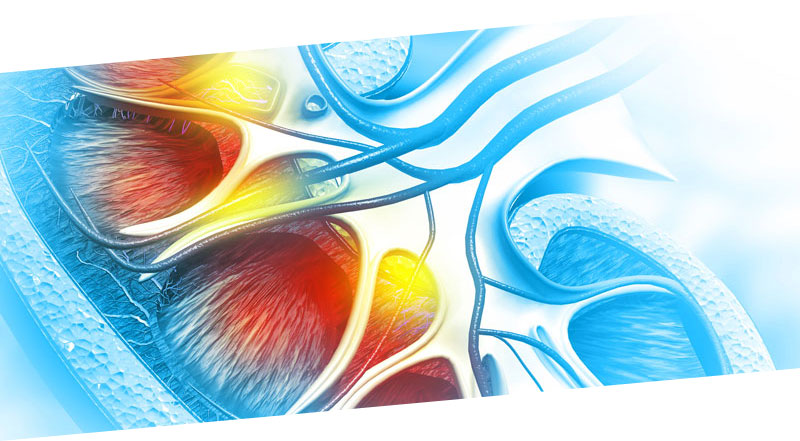
The two diseases that comprise C3G both involve a high presence of a protein called C3G in the renal glomeruli. The glomeruli are the filtering units of the kidney.
In patients with C3G, proteins in the blood get broken down in such a way that breakdown products get lodged in the kidney, setting off reactions that injure the glomeruli. Injured glomeruli can’t filter blood as well, which hampers urine production. As this continues, toxins build up and damage kidney tissue.
What are the symptoms of C3G?
Common symptoms of C3G include:
- Blood in the urine (hematuria)
- Excess protein in the urine (proteinuria), evidenced by dark, foamy urine
- Reduced glomerular filtration rate (GFR; reduced ability of the kidney to filter the blood and make urine), elevated creatinine
- Fatigue
- Swelling (edema) of hands, feet, and/or ankles
- High blood pressure
- Decreased urine output
How is C3G diagnosed?
Doctors may order a urine test to check for proteinuria and hematuria. A blood test can measure serum creatinine levels; unusually high levels may indicate kidney damage. A blood test can also reveal glomerular filtration rate (eGFR), which shows how well the kidneys filter waste from the body. C3G disease severity depends on low eGFR and high proteinuria.
The only way to diagnose C3G specifically, however, is with a kidney biopsy. Kidney deposits stain for the complement protein C3. When examined under an electron microscope, the doctor can see breakdown deposits indicative of C3G.
How is C3G treated?
While there is no treatment for C3G, certain steps can help slow the progression of kidney damage over time.
Blood pressure and cholesterol medication is a good start. Angiotensin converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARBs) both control blood pressure as well as reduce the amount of protein in urine.
Controlling high fat lipids (cholesterol) in your body helps reduce kidney damage as well as lower heart disease risk. Reducing sodium content and protein in the diet may also reduce stress on the kidneys.
Studies suggest that mycophenolate mofetil (MMF) can decrease the rate of kidney damage in patients with C3G. A study out of Oregon Health Science University in Portland, Oregon, found that MMF combined with corticosteroids induced remission in 67% of the 30-patient cohort.
Another study looked at the effect of MMF on Southeast Asians with C3G. After six months of therapy, 23% of the patients (4 out of 17) showed complete remission, or a return of serum creatinine levels to baseline. Seven patients (41%) achieved partial remission.
Eculizumab (Solaris®), a drug designed to treat rare blood disease, may be effective in slowing proteinuria and kidney disease progress, but it only works about 50% of the time according to nephrologist Paolo Cravedi, MD, a nephrologist for Mt. Sinai, commented in an article for Pharmaceutical Technology.
Biorasi currently finished 12 to 16 months of enrollment in a rare kidney disease C3G phase II study to evaluate the safety and biologic activity of a new drug. Biorasi has 19 nephrology (kidney) clinical sites.
We know people affected by C3G need better treatment options. It is a disease with unmet medical needs that tends to manifest in childhood.
As a CRO that understands the challenges involved in researching rare disease treatments, we’re here to help drug developers deliver the most effective clinical trials possible—on time and on budget.
Speak with one of our rare disease experts today to find out how we can help you develop your next rare disease program.